COVID-19 Makes Promoting Well-Being Resources More Important Than Ever
The COVID-19 health emergency has once again highlighted the value of well-being. During the COVID-19 pandemic, many aspects of normal work, including promoting well-being resources, may have taken a backseat. The immediate focus for communications shifted to how to avoid getting COVID-19 and what to do if you get it. As the health emergency evolves, and we shift again to living and working with fewer restrictions (while still maintaining safety measures), employers and plan sponsors need to adapt yet again. Shelter-in-place mandates and the fear of venturing out caused many to delay routine checkups. New questions have emerged about the long-term cost of deferred care.
While there are many factors that can lead to the quick spread of COVID-19—including lack of access to clean water, living in close quarters to others, limited access to grocery stores and nutritious food, working on the front lines, and challenges to accessing care—if you review data on outcomes from COVID-19 cases to determine who recovers quickly, who becomes severely ill, and overall survival rates, a general pattern seems to emerge. Those in good health have fewer complications and less risk. For example, ICU admissions for COVID-19 are linked to chronic diseases, such as diabetes and hypertension. As the risk of COVID-19 infection persists, maintaining one’s health and well-being remains key to virus prevention—and has taken on increased importance during a time wrought with challenges to physical, mental, and financial health.
Healthy habits, including good nutrition and frequent physical activity, are the first steps in protecting your health and staying well. Promoting these and other beneficial activities is the foundation of any well-being campaign or wellness program. Chronic diseases (diabetes, heart disease, and lung disease) account for 86% of health care costs. Several research studies, including one from the Cleveland Clinic, have linked lifestyle risks to most chronic conditions, including those that increase risks related to COVID-19. Many of these chronic diseases are preventable and/or manageable with the adoption of a healthy lifestyle.
Wellness programs can be geared toward adopting healthy lifestyles that help manage chronic conditions and yield positive outcomes. Through wellness programs, individuals can improve their health while health plan sponsors experience reduced health care costs.
Employers and plan sponsors offer valuable resources that their people—and their people’s families—can use to prioritize their health. Your people have a lot on their plates and minds right now: juggling kids, elderly loved ones, and work; dealing with financial issues; worrying about loved ones; and grieving. These challenges underscore the need to continue communicating about the benefits that can help them manage through this crisis. Reminding your people about where to find and how to access well-being resources may help people prevent or reverse underlying conditions that make COVID-19 so devastating. In this climate in which the value of well-being has again been underscored, employers are reminded that promoting well-being benefits is more important than ever.
The Connection Between Chronic Diseases and Severe Cases of COVID-19
According to a recent CDC report, 32% of Americans who have died from COVID-19 have diabetes. That’s almost three times the percentage of diabetics in the population (about 11%). Lung disease—specifically, asthma and chronic obstructive pulmonary disease (COPD)—affects 13% of the population but is linked to 21% of COVID-19 deaths.
Age is often mentioned as a risk factor for COVID-19. That may be attributable to higher incidence of diseases, such as diabetes, lung disease, and cardiovascular disease, among older adults.
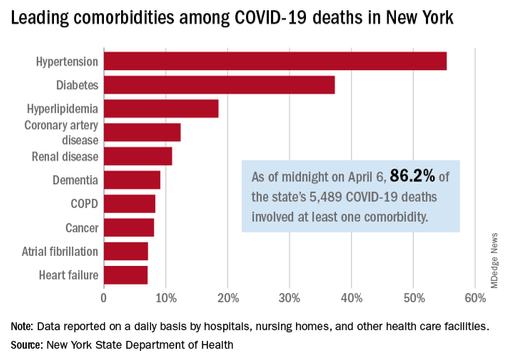
Among the non-elderly, early data emerging from analyses of COVID-19 cases indicates the large majority of the deaths occur in patients who have underlying diseases (comorbid conditions). Based on existing data, all these conditions are associated with an increased risk of an adverse outcome: cardiovascular disease, hypertension, COPD, severe asthma, diabetes, kidney failure, severe liver disease, immunodeficiency, and malignancy.
Leading comorbidities among COVID-19 deaths in New York
The difficult outcomes we have seen occur in our nation may leave us with a sense of loss, anxiety, and fear, to name a few emotions. While we cannot turn back and erase the experiences of those who have suffered, we are reminded that each individual holds the power to influence outcomes related to his or her own health in the years ahead.
We’ve again been shown through the data of this health emergency that healthy people of any age group have a lower risk of poor outcomes (in this case related to COVID-19) than do their peers of the same age who have one or more comorbid conditions. Individuals who work to maintain their well-being will reap benefits now and in the future. Employers and plan sponsors can support this through promoting well-being resources and thoughtfully designed wellness programs.
Mental Health, Substance Use, and COVID-19
The social isolation and stress caused by COVID-19 containment measures are raising serious concerns about implications for mental health. New or managed conditions may be escalating. Questions abound, such as whether those developing new conditions are seeking treatment and whether those in a current course of treatment are finding challenges in transitioning to alternative methods for accessing care. The necessary COVID-19 containment measures, like sheltering in place and quarantining, used to prevent the spread of COVID-19 may be increasing substance abuse.
According to the National Institute on Drug Abuse, while little is known about COVID-19 in relation to substance use, there are potential associations between severe COVID-19 cases and substance-use disorders. People who have opioid-use disorder (OUD) may have a harmful decrease in oxygen in their blood (hypoxemia). That diminishes lung capacity, which puts them at higher risk of having a severe case of COVID-19. Methamphetamine users are also at high risk, because that drug constricts the blood vessels, contributing to pulmonary hypertension, which increases the impact of COVID-19.
Wellness programs can help people seek care, keep up with their treatment regimen, or access social supports related to their needs. Promoting activities that lead to a healthy lifestyle—including exercise and getting outdoors—can also boost mental well-being.
Emphasize Wellness to Promote Physical and Mental Well-Being
In the absence of a vaccine or a cure, we’ll be living with COVID-19 for quite a while. Given the adverse impact of COVID-19 on those with physical and mental health comorbidities, well-being and mindfulness are of paramount importance now and for the foreseeable future.
People who commit to improving their health—even those with existing chronic conditions—will give themselves the best chance to reduce their risk of hospitalization and death from COVID-19 and other calamities. They can take control over their well-being by adopting a healthier lifestyle. Plan sponsors play a key role in bringing awareness to well-being resources and can continue to serve as leaders in this effort, knowing the long-term benefits to their people and their families.
Clearly this is a good time to (re)start or (re)promote your wellness program! You have a captive audience who’s likely to be receptive to your messages.
Work with Us
We partner with organizations that value their people first. Let’s talk.

SVP National Medical Director Segal